What is Myofascial Pain Dysfunction (MPD)?
Myofascial pain dysfunction (MPD) refers to pain and inflammation in the body's soft tissues.
MPD is a chronic condition that affects the connective tissue that covers the muscles. It may involve either a single muscle or a muscle group. In some cases, the area where a person experiences the pain may not be where the myofascial pain originated. Experts believe that the actual site of the injury or the strain prompts the development of a trigger point that, in turn, causes pain in other areas.
Myofascial pain may result from acute muscle strain or from chronic over-use or misuse (i.e., misalignment of upper and lower teeth, teeth grinding, teeth clenching, poor posture, anxiety or stress, fatigue)
TMJ and myofascial pain syndrome
In addition to pain, muscles may exhibit restriction in range of motion or loss of strength. Since muscle spasms (myospasms) produce pain, which in turn produce more muscle spasms, the resulting cyclic condition can continue indefinitely, even after the original cause of the muscle spasms has been resolved. The term used to describe this condition is Myofascial Pain Dysfunction Syndrome (MPD) and will usually not resolve without appropriate therapy.
Cervicogenic Pain
Most people will experience neck pain during their lifetimes, but this will not typically interfere with daily life. However, there is a significant coexistence of neck pain and TMD. This can be traced to the anatomy of the neck and jaw and the high level of interaction of the bones, muscles, ligaments, and nerves between the two. Much as neck muscles do not contract independently, neck and jaw muscles do not contract independent of each other. Loss of function, or dysfunction, in one group is compensated for by other muscles, consequently setting the stage for patients to experience pain in these areas. Further complicating this issue is the concept of referred pain, which is a significant issue with neck and TMD pain. This is due to the merging of nerves from these related structures in the head and neck, and sometimes even a widespread pain condition leading to pain in multiple muscle groups in the region.
These issues can stem from an acute injury, but may also develop over time and become a chronic issue without an accompanying injury to explain the presence of the pain. Therefore the diagnosis patients with TMD must involve examination and consideration of the neck structures to develop a proper treatment plan. This is best managed by a physical therapist working in conjunction with the orofacial pain doctor.
Trigger Points (TPs)
Prevalence: TPs are extremely common and will likely affect nearly every one of us at one time or another. If you have ever had a “stiff neck” or a “back ache” you have experienced what an active TP feels like.
A muscle cane be inflamed, injured, even physically injured (tear; strain) but these conditions are far less common than muscle pain to to the presence of a TP. To be certain that we are dealing with muscle TPs, following essential characteristics must be present: 1) tender spot in a taut band" of muscle, 2) painful limited range of movement, 3) predictable pattern of referred pain with palpation of the taut band and 4) when palpated or provoked the TP will cause the muscle to “twitch” called a twitch-response.
TPs can be latent or active: 1) latent TPs can merely cause stiffness and restricted range of motion without pain and, 2) active TPs which can cause severe, debilitating pain interfering with the quality of daily life
Common symptoms when TPs form: TPs often begin to develop in the muscles if the nearby temporomandibular joint (TMJ) is not functioning normally. Most patients will report clicking, popping, and/or locking of the TMJ. The TMJ can become inflamed resulting in local pain which is often experienced as “earache”. Many patients often feel that the “bite feels off” and that it is more “difficult to close on the back teeth” and that they are now “contacting more on the front teeth”.
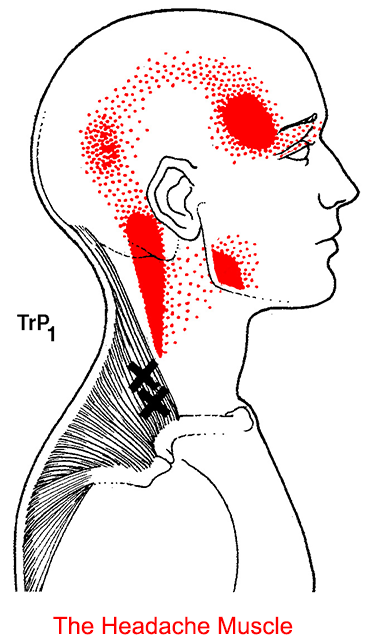
Referred pain from TPs: if the TPs are persistent, inflammation can begin to accumulate leading to pain which often causes the associated nearby muscles to tighten up and stay tight until the joint problem is addressed. This sustained guarding reaction of the muscles is known as Protective co-contraction can remain constant leading to This constant guarding or “protective” reaction by the muscles has been shown to lead to the development of painful active TPs. Below is a diagram displaying areas of referred pain we often see in TMD patients:
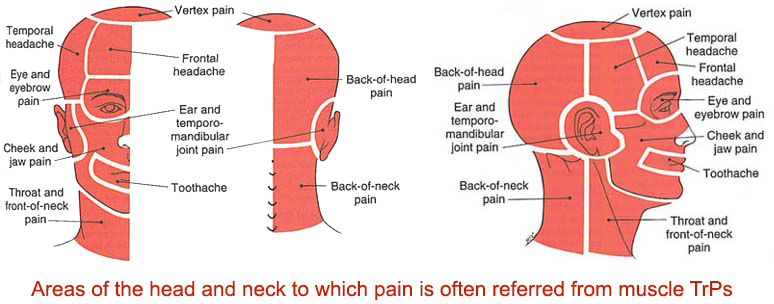
Examples of Referred Symptoms from Muscles with Active Trigger Points (click to enlarge):


TMD: The Great Imposter: TPs can persist for weeks, months, or even years, and mimic a number of medical and dental conditions. Many of our patients report that have been unsuccessful in controlling their pain from treatments such as: 1) migraine medications, 2) trigeminal neuralgia, 3) orthodontics therapy 4) bite adjustments, 5) TM joint surgery, 6) night guards (often for many years), 7) multiple medications / pain management to name a few.
Additional symptoms: Other symptoms often reported from TPs which remain untreated: TPs which are particularly active will cause constant deep pain which can cause excitation or stimulation of neighboring nerves which bombard the brain leading to very aggravating symptoms such as: 1) dizziness, 2) sinus symptoms, and 3) toothache.
Perpetuating Factors: some common conditions which interfere with the patient’s ability to respond to treatment which may need to be addressed and are called Perpetuating Factors (PFs). Common PFs are: 1) Sleep disturbances are common problems affecting nearly 47% of TMD patients. Sleep-related breathing disorders (snoring; obstructive sleep apnea), 2) Movement disorders such as Restless Legs Syndrome & Periodic Limb Movement Disorder, 3) Low vitamin D levels, 4) Chronic emotional distress, anxiety, and depression, 4) Chronic physical stress such as daily computer or telephone work without much of a break, 5) physically deconditioned/disabled 6) Metabolic deficiency such as a low or low-normal functioning thyroid gland.
Controlling or eliminating PFs can mean the difference between success and failure so the fact that one has “always had a sluggish thyroid” does not mean that it does not need to be addressed at all! If therapy eliminates your pain but recurs over and over again, this is an indicator that PFs are in effect. Muscles that are hyperirritable because of less-than-optimal health will not respond well to therapy no matter how often the treatment is repeated.
